Venous Insufficiency: Why Your Veins Struggle to Return Blood to the Heart
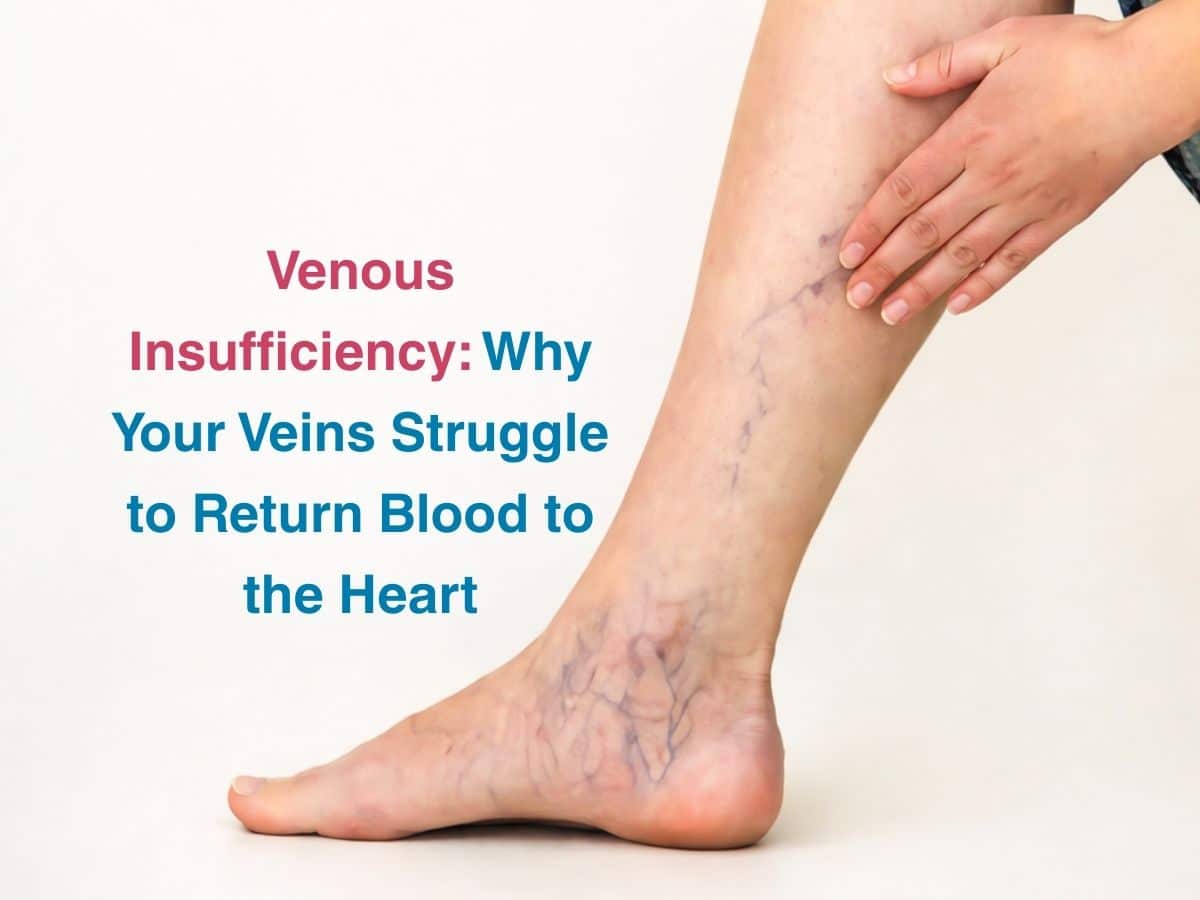
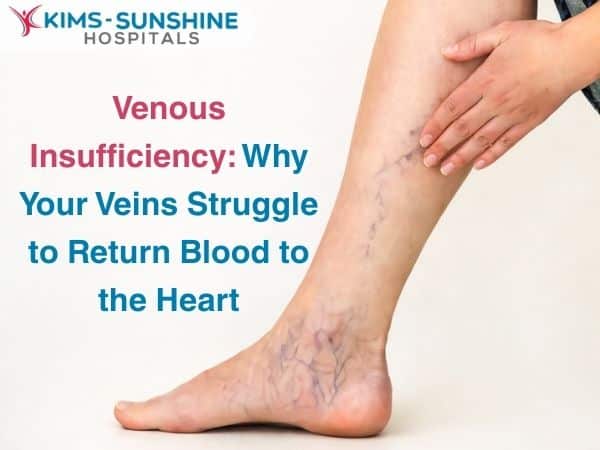
Venous insufficiency is a condition that affects millions of individuals all over the world, including in the Indian subcontinent. It tends to affect more women than men for some reason though population studios are still being done to understand the prevalence of this condition better. Venous insufficiency is mostly a chronic condition, which is why it is termed CVI- where the valves that are present in the veins of your legs do not work like normal- causing blood to NOT flow back to the heart in a systematic manner. This can lead to symptoms which are painful in the long run. Since blood is not able to move back up into the heart, it tends to pool in the legs itself leading to greater blood pressure in those blood vessels. This can lead to damage to the venous walls. Varicose veins and spider veins are a common side effect of CVI.
Causes of CVI
Chronic Venous Disease is a common condition that affects one in every 20 individuals worldwide. It is mainly caused by congenital defects – where people may be born without valves in their veins. For others- it may be because of the vein getting too large in size- so even if the valve is working properly, backflow cannot be prevented. This is called a primary cause for CVI. A secondary cause is when CVI is occurring due to a condition like deep vein thrombosis- where a clot can form and damage the valves of the veins.
Venous Reflux Symptoms
Some common signs and symptoms associated with this condition include
- Tingling or burning sensation in the legs
- Your legs may ache or feel tired
- Skin looks discoloured
- You may notice cramping at night
- If you stand for a long time- then you may notice fluid accumulation
- Ulcers may also form in severe cases of CVI
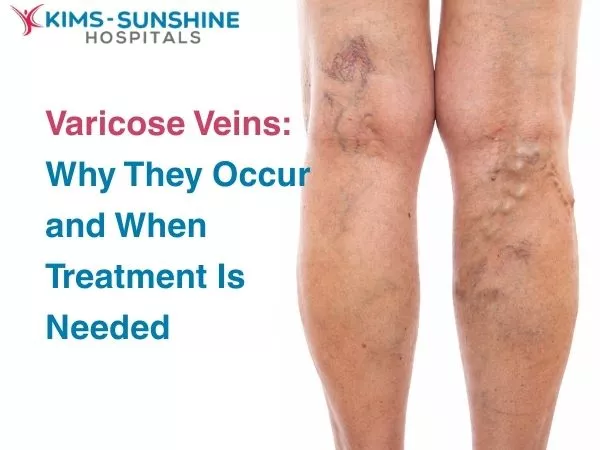
Varicose veins are common and can predate this condition.
Venous disorders are ranked into different stages- depending on severity of symptoms. It starts from Stage 0 and goes up to Stage 6- where it begins at 0 with cramping or tired feeling legs and ends with an active ulcer that has formed (in stage 6). CVI is diagnosed if you have crossed stage 3 – where you notice varicose veins and oedema, or even skin related changes at times.
Vein Ultrasound Diagnosis
Apart from a detailed visual and physical exam – to check how your blood vessels in the legs look – like skin colour, presence of varicose or spider veins, a vascular ultrasound is the best way to check how blood flow is occurring in the affected region. This will also tell your doctor which veins are damaged and extent too. Some people may have both CVI and peripheral artery disease (PAD)- in which case additional care must be taken to prevent compression of blood vessels in the legs.
Venous Insufficiency Treatment
Treatment approaches normally focus on helping you deal with symptoms- like making blood flow better using anticoagulants, treating ulcers, reducing pain and swelling and helping with any skin issues. You should focus on maintaining a normal weight as being overweight can place extra stress on these blood vessels. Compression therapy with stockings is also recommended at times but this is not always the case if you have both CVI and PAD. Antibiotics are used to help deal with ulcers, if they have been infected. Non-surgical treatments include sclerotherapy and thermal ablation of affected large veins- where heat is used to destroy it, minimising scarring and bruising. Surgical treatment is recommended if no other approaches have worked- like stripping, vein bypass or removing the problematic veins. Vein bypass involves taking a stretch of healthy vein and using that to replace the affected vein in the part of the body showing symptoms.
Conclusion
Since this is a chronic condition, long term management is essential- you need to ensure that ulcers don’t form, and if they have – they need to be treated without any delay. Eating well, getting enough physical exercise and managing your weight and also taking medications to manage any underlying conditions can help you stay symptom free for the most part. Don’t sit or stand for too long and watch how your skin looks everyday.