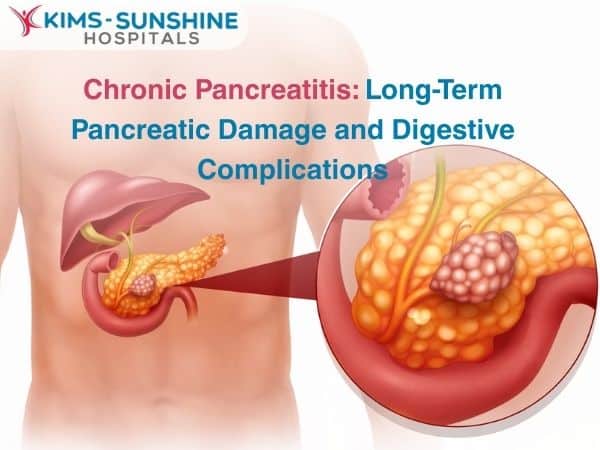
Chronic Pancreatitis: Long-Term Pancreatic Damage and Digestive Complications
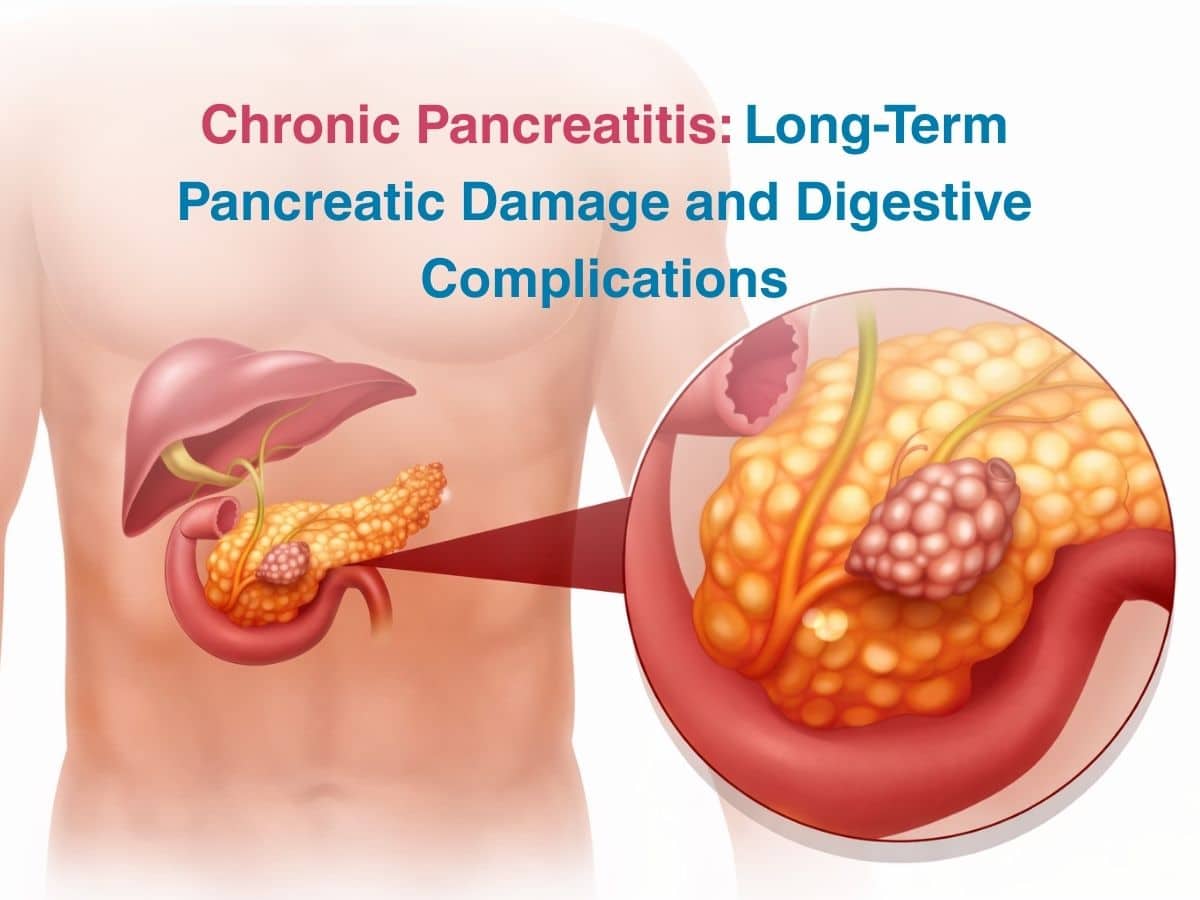
When the pancreas gets inflamed due to any underlying cause or injury, it can interfere with how your body metabolises certain foods like sugars and proteins, as insulin and amylase are produced by specialised cells in this organ. Inflammation of the pancreas can cause severe abdominal pain and cause issues with regulation of blood glucose levels, if not addressed promptly. While inflammation itself as a process occurs as a response to injury, continually high levels of it can affect the functioning of organs and systems in the long term. Chronic pancreatitis can be a lifelong condition which can get worse if not managed in the right way. Acute pancreatitis on the other hand can be observed with a sudden onset of symptoms like pain due to a short term injury of some sort.
Causes for Pancreatitis
Some of the main causes for this condition include-
- Chronic or long term exposure to alcohol- Alcohol-related pancreatitis can damage tissue and cause inflammation which can lead to fibrosis (which is when severe inflammation can lead to the formation of scar tissue). This can cause pancreatic enzyme deficiency as the organ is not able to function normally. But the exact mechanism as to how pancreatic tissue gets inflamed due to alcoholism is still being studied by researchers.
- Gallstones– when the bile duct gets blocked due to the presence of a gallstone, it can slow down or completely stop the flow of pancreatic juice into the small intestine. If the stone remains there for long, the enzymes from the pancreas begin to digest the tissue itself- resulting in loss of function of the pancreas. This is why gallstones are a leading cause for pancreatitis.
- Other causes include viral infections, autoimmune disease of some kind, cystic fibrosis, ischemia in the pancreas, cancer or any kind of traumatic injury, which can harm pancreatic tissue.
- Some cases of pancreatitis are idiopathic too- but this is very rare. In such cases, no underlying cause can be pointed to, but the pancreas remain highly inflamed and its function gets compromised.
Symptoms of Pancreatitis
Chronic abdominal pain is a major symptom of this condition. Acute pancreatitis can also cause symptoms like shallow breathing, palpitations of the heart, fever and leave you feeling very nauseous.
Chronic pancreatitis can cause weight loss, poor appetite, low blood pressure, indigestion and fatty stool.
Pain in the abdomen is common but the severity and location can vary. The pain may also radiate to the back for some people. Others deal with constant pain which may be mild, or others say that it comes and goes. When the pancreas is not able to function for prolonged durations of time, it can begin to cause malabsorption symptoms like very smelly stool, chronic diarrhoea, unnecessary bloating after a meal and even weight loss, since it is hard for you to feel comfortable after a heavy meal. When this continues, it can slowly begin to impact how other organ systems function.
Diagnosis of Pancreatitis
Apart from a medical history, blood glucose tests are taken to check glucose levels and insulin activity. Your stool is also a valuable sample to test for the presence of undigested fat or if enough digestive enzymes are being made by the pancreas (specifically stool elastase) respectively. Other blood tests check for any nutritional deficiencies. Imaging is also very helpful in diagnosis- a CT scan for pancreatitis or even an MRI can show if there are any structural abnormalities in the pancreas.
Treatment of Pancreatitis
Supportive care like fluids, rest, parenteral nutrition and pain relief are recommended for acute cases of pancreatitis. If a gallstone is the culprit, surgical removal of the stone and the gallbladder may be done. The surgery can be done laparoscopically or with traditional open surgery.
Chronic pancreatitis management will involve a more involved strategy where you make changes to your daily routine, take medications and painkillers to manage symptoms and use insulin injections to help your body metabolise glucose better.
Conclusion
Since digestive enzymes are not being made normally, nutrients won’t be absorbed efficiently by the small intestine. You will hence be asked to take supplements to combat any nutritional deficiencies. Very severe cases of pancreatitis can mean the necessity for surgical removal of the pancreas- a part or the whole. In such instances, you will need to take insulin and other digestive enzymes with your meals for the rest of your life. Talk to an experienced gastroenterologist at KIMS Sunshine Hospital, so you can understand how to take better care of yourself. Learn how to make sustainable changes to your lifestyle in the long term after you talk to us!