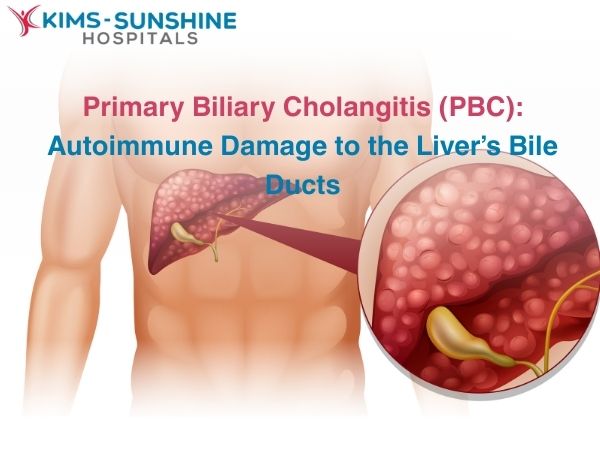
Primary Biliary Cholangitis (PBC): Autoimmune Damage to the Liver’s Bile Ducts
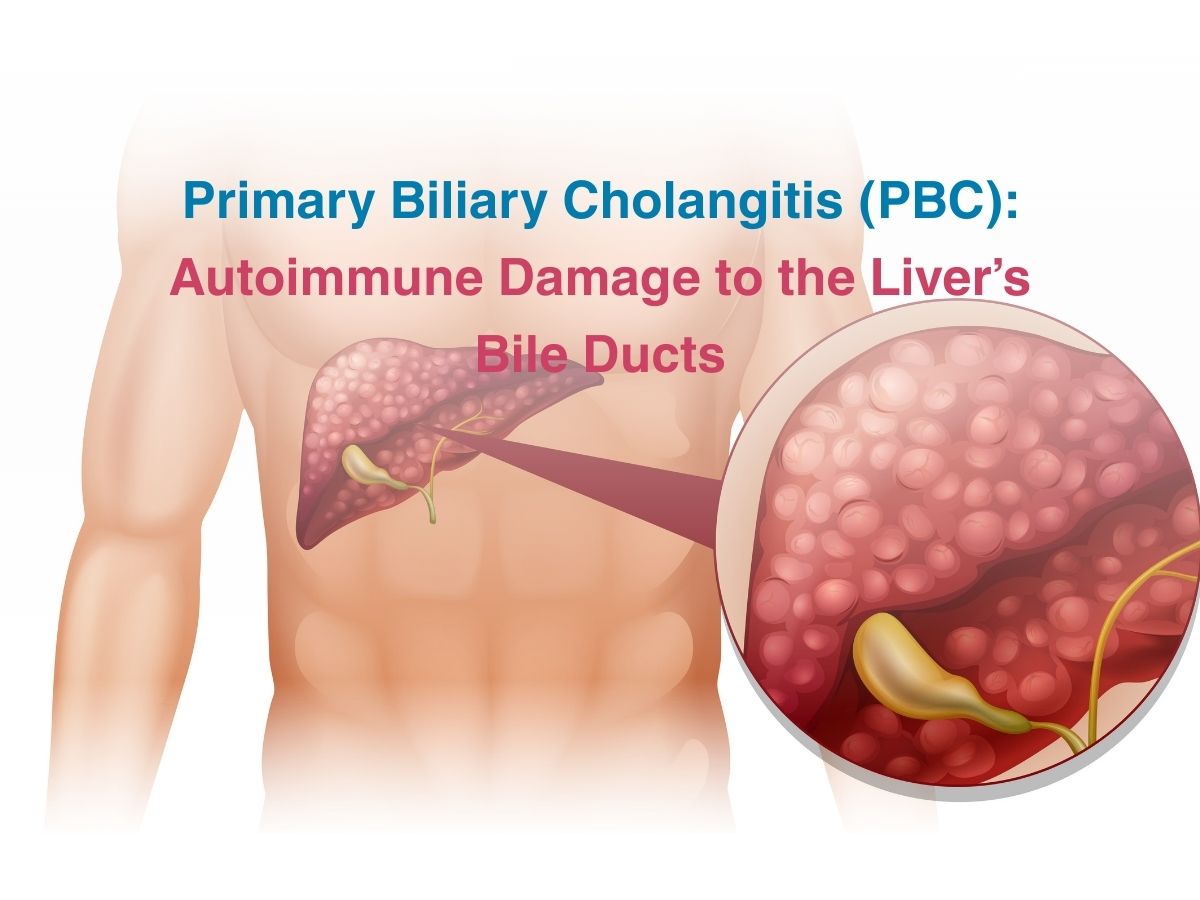
The liver is the largest organ in the body which serves multiple functions in the body. One of them includes its ability to produce bile – a yellow coloured fluid that contains salts which help break down fats in the small intestine, It also serves as a means for wastes to get excreted out in the faeces. Bile flows through specific channels called the bile ducts and it is these ducts that get chronically inflamed, causing biliary cholangitis. It is termed primary biliary cholangitis (PBC) when there is no specific reason for the inflammation – which is also why the process continues and does not know when to stop. If the bile has nowhere to go, it remains in the liver and begins to cause issues which can culminate in liver failure.
Causes and Symptoms of PBC
Chronic bile duct inflammation can lead to liver failure, if not managed in the long term. The main reason for PBC is an overactive immune system which begins to attack the liver duct cells. Studies have shown that there are a few genes which can increase the risk of this happening. Other individuals have had viral infections which were not taken care of in time and that triggered their immune system to cause issues later on. Inflammation mainly depends on triggers and these can be genetic, infection based or even from exposure to a particular compound in the environment.
Symptoms of PBC include
Itchy skin and extreme fatigue present in the majority of the cases. The initial signs are subtle and hence easy to ignore. Another major problem is malabsorption of fat by the gut. This can lead to high cholesterol levels in the blood, fatty poop, diarrhoea, nutritional deficiencies in fat soluble vitamins like D, A and K, or even osteoporosis in the long term due to a marked reduction in Vitamin D values.
The increasing levels of inflammation in the bile ducts can cause scar tissue or fibrosis to occur- which can harden the blood vessels in the liver and lead to hypertension. Portal vein hypertension can cause cascading effects in the system- like an enlarged spleen, liver, poor immunity, swollen veins, spider angiomas, GI bleeding, fluid build up in the abdomen and even severe confusion in extreme cases, due to the high amounts of toxins found in blood.
PBC affects more women than men. PBC symptoms in women include- dry, itchy skin, severe joint pain, skin colour changes, autoimmune issues and extreme bouts of fatigue which can hamper their daily quality of life severely.
Diagnosis of PBC
Apart from a detailed physical exam, imaging and other blood tests will be conducted to diagnose liver specific conditions. Elevated alkaline phosphatase levels in blood can point to liver stress. Since liver cells are very metabolically active and are heavily dependent on good mitochondrial activity, blood tests check whether the immune system is making proteins to attack those specific mitochondria- this test is called the Anti-mitochondrial antibody (AMA) test, which is an indicator for PBC.
An MRI may also be done to check for any swelling or structural abnormalities of the liver. Some individuals may have PBC but still test negative for AMA, so in such cases, a liver biopsy is used to confirm the condition.
Treatment for PBC
There is no cure for this condition, but Ursodeoxycholic acid treatment (UDCA) is a kind of bile salt that is used to get rid of bile from the liver and prevent liver damage. But, it is more effective when PBC is caught in the early stages. For others who don’t do well with UDCA, obeticholic acid may be prescribed. Doctors may try to regulate your immune system by prescribing antihistamines, UV light therapy and also give you supplements so you won’t suffer from nutritional deficiencies.
If nothing works and liver failure has progressed to a very severe level, liver transplantation surgery may be carried out. Most individuals do well after a transplant, though their immune system may begin to attack the new liver too, later on. But, the progress of the disease is much slower and is hence easier to manage.
Conclusion
Primary biliary cholangitis is a chronic liver disease which only gets worse with time. It hence needs to be managed effectively with medication and by making sensible changes to your diet and lifestyle. You should aim to eat fresh produce, avoid smoking and drinking, eat less fatty foods and ensure that you get enough exercise on a regular basis – like a brisk walk and some resistance training to help preserve bone and muscle health. Dealing with PBC involves staying in touch with experienced specialists. Come to KIMS Sunshine Hospital, so you can talk to a hepatologist and get the advice and treatment you require, today!