Nocturnal Hypertension: Why Blood Pressure Rises During Sleep and Why it Matters
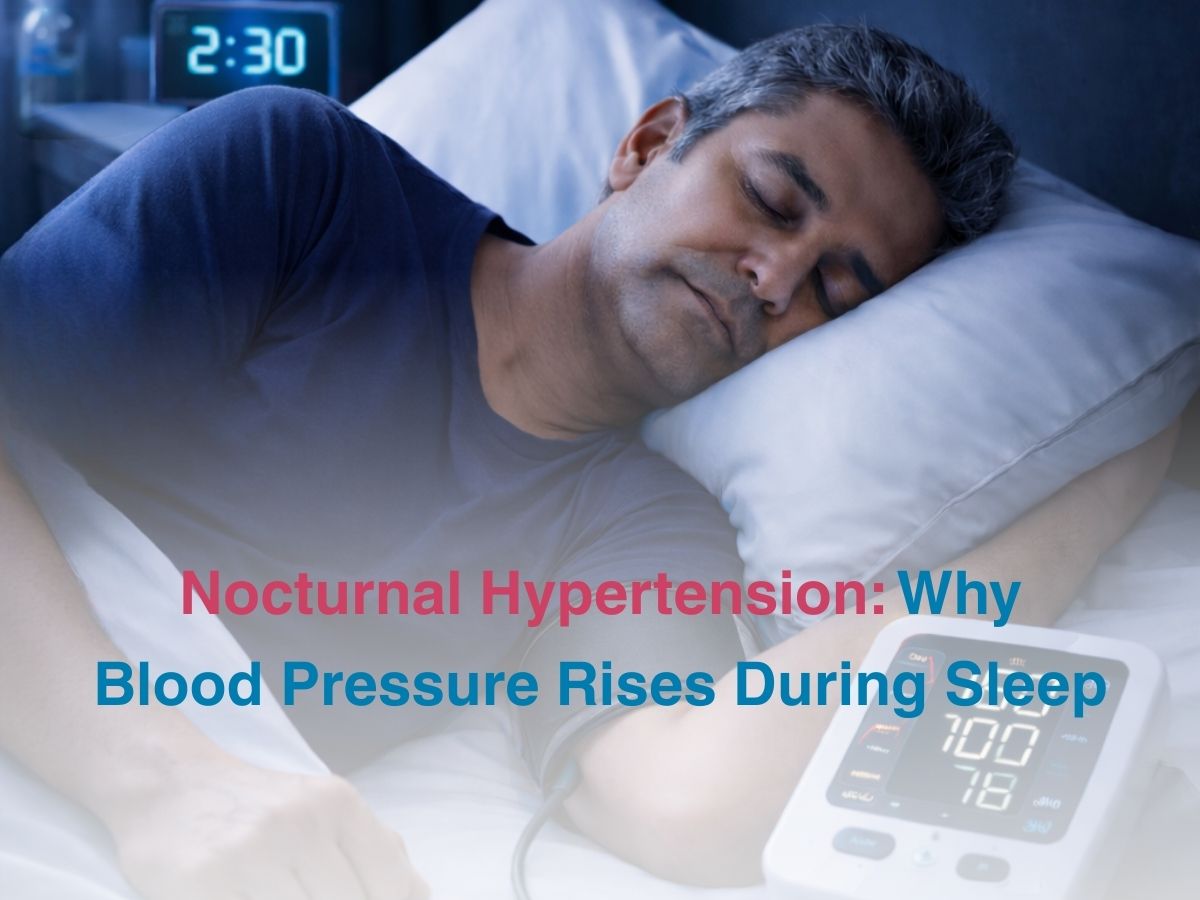
We usually talk about blood pressure as though it is affected only during the day. Stress, physical exertion, emotional strain and diet are blamed for high BP levels but we don’t understand the fact that our blood pressure follows a rhythm just like the rest of our bodies, which continues through sleep, not just when we’re awake. In healthy people, BP naturally drops at night, just to give their hearts and blood vessels some time to rest. This drop is known as nocturnal dipping and is an important marker of cardiovascular health. In some people, this rhythm gets messed up. Blood pressure rises, instead of dipping. This condition is called nocturnal hypertension and since it happens when you’re asleep and all routine measurements are made during the day, it goes unnoticed. This condition has been recognized as a major risk factor for conditions like heart disease, stroke and kidney damage. Understanding why blood pressure can act differently at night can help us maintain our long-term cardiovascular health.
What Is Nocturnal Hypertension?
Nocturnal hypertension just refers to elevated BP, when you’re asleep. It is identified through a method called 24-hour ambulatory blood pressure monitoring, not standard clinic readings. For most of us, BP drops by around 10-20% when we’re asleep. When this doesn’t happen, the person is called a “non-dipper.” When BP rises during sleep, it’s called reverse dipping. Nocturnal hypertension is not the same as hypertension during the day. You could have normal or mildly elevated BP during the day and still have a significantly higher level while asleep. This could result in the condition being hidden in plain sight for years, silently damaging your blood vessels and organ systems. Research shows that measuring BP elevation while sleeping is a better predictor of cardiovascular health than BP readings taken during the daytime. Due to the reasons we’ve mentioned, nocturnal hypertension is being viewed as a distinct and clinically important condition now. It’s not a variation of standard hypertension anymore.
What Disrupts Sleep-Dipping?
The normal drop in BP while sleeping is regulated by synergy between your nervous system, hormones and sleep cycle. During deep sleep, your sympathetic nervous system becomes less active and this lets your blood vessels relax, your heart rate slows down and your BP reduces. While this is happening, your parasympathetic nervous system starts getting more active and this directly supports rest and recovery. Hormones that are responsible for or affect your BP follow your circadian rhythm. Cortisol raises BP and blood sugar and is at its lowest level at night. Melatonin supports sleep and helps relax blood vessels. It’s at its highest while you’re asleep.
Both of these hormones create a safe environment in your body, so your BP can dip. Sleep disorders like sleep apnoea can interfere with this process. Sleep apnoea triggers stress responses which can cause sharp rises in BP multiple times when you’re asleep. Chronic stress and irregular sleep cycles can also disrupt normal regulation. Other factors like obesity, diabetes, chronic kidney disease, smoking and drinking can also contribute to this condition. Nocturnal hypertension is mostly never just an isolated problem, it tends to point to broader issues.
Health Risks And Early Detection
Nocturnal hypertension basically strains your cardiovascular system continuously when it’s supposed to be resting and your body is supposed to be recovering. Persistent elevation leads to faster damage of blood vessels and increases load on your heart. Over a period of time, this can lead to actual structural changes to your heart muscle, like thickening of the walls. This just raises the risk of heart failure. The brain and kidneys are also very vulnerable to these elevations. The kidneys rely on stable blood flow for filtration and may suffer irreversible damage when exposed to wobbly BP levels with multiple elevations during the night. Early detection can help you treat this condition by treating underlying sleep disorders, adjusting your lifestyle and sleep cycle, before it leads to long term complications.
Conclusion
Nocturnal hypertension is a condition that’s regularly overlooked when talking about blood pressure regulation. Since blood pressure doesn’t decrease when you’re sleeping( as it normally should), your cardiovascular system is under continuous strain. Routine measurements are usually taken during the day, so this condition can remain hidden until it leads to a severe complication. Early detection and intervention is better than treating whatever complication may arise later.