Hypercoagulability: Signs, Risks, and How to Prevent Thick Blood Issues
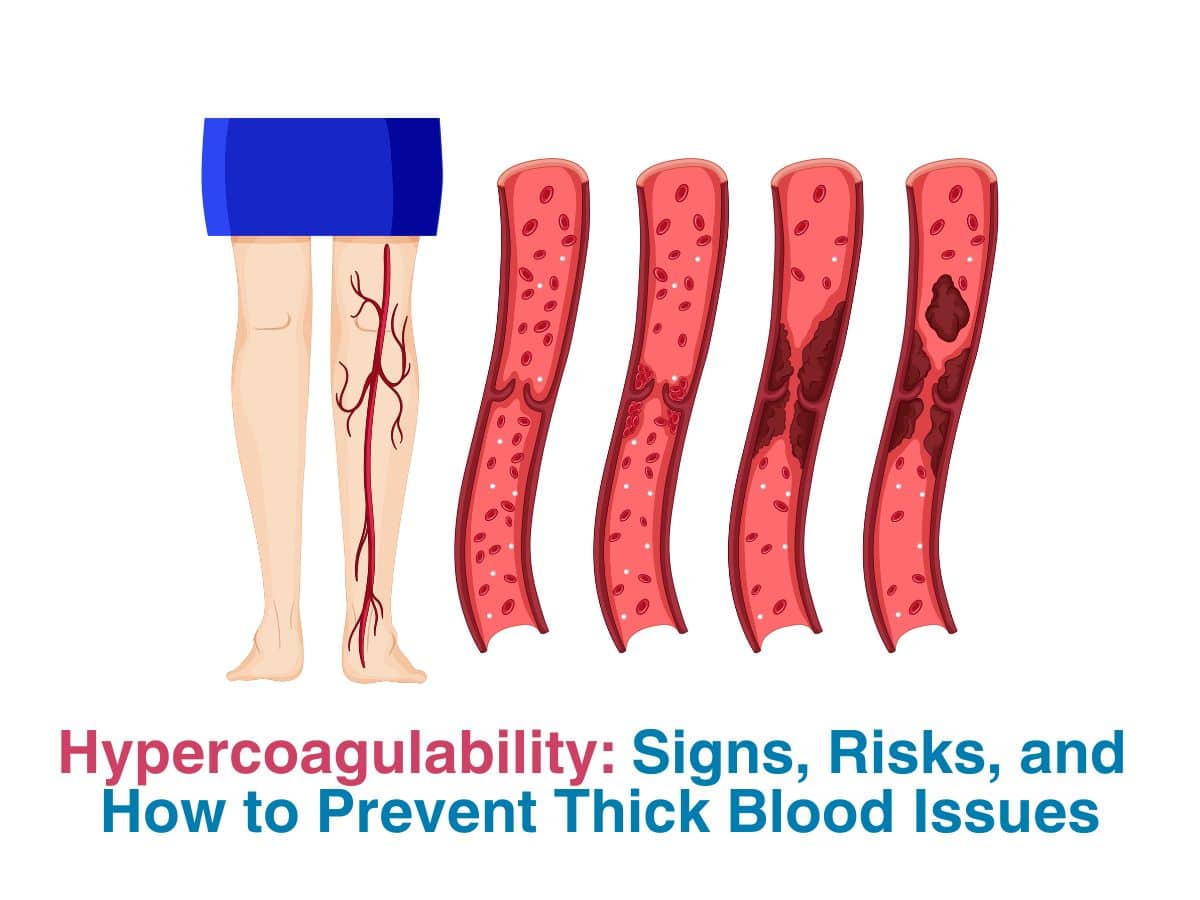
Your blood needs to remain a runny fluid, so it is easy to circulate all over the body and provide nutrition to each and every cell. Your blood also has this crucial ability to clot or thicken when there is any injury involved. The clotting only happens in rare instances, with the help of specific proteins called ‘clotting factors’. These remain inactive, unless there is injury, in which case, they become active – to reduce bleeding. If you however have one of these clotting disorders like hypercoagulability, then you need to be careful, as it is a condition where your blood clots in seemingly normal conditions, even when you don’t have an injury for instance. Blood clots normally aren’t a huge issue as they go away but if they are big, then it may cause blood flow to stop- leading to conditions like a heart attack or a stroke.
What Causes Blood To Become Too Thick?
We used terms like hyper and coagulability above. On a normal day, your blood just seemingly minds its own business, flowing around with ease. But, if you have faulty genes causing a clotting disorder, then your blood may not be as runny anymore. This is because it will coagulate or thicken or solidify, even when there is no need for it to happen. A clot is also called an embolus or thrombus. These ‘clots’ can cause issues like Deep Vein Thrombosis (DVT) or a pulmonary embolism (clot in the lungs), and can cause restricted blood flow to your limbs- leading to severe cramping and pain, or even a stroke in extreme cases. If you have a clotting disorder and are pregnant, then it will be treated as a high risk pregnancy- mainly to prevent a miscarriage from occurring. This condition is not so easily found in India- either due to it being underreported or it genuinely being lower in number than the west.
Early Signs And Symptoms Of Hypercoagulability-
Let us look at the early signs and symptoms you need to watch out for, as most of us are not very aware of our genetic makeup.
- If you feel short of breath even after breathing in deeply
- If you have random but severe headaches
- If you have pain in an arm or leg – along with tenderness and redness
- If you have stroke-like symptoms- like vision change, one side of the body not working well, or dizzy- then get help ASAP!
It is important to remember that the symptoms will vary, depending on where the clot is formed. The symptoms may seem to change- which means the clot is moving around. If it is the brain- you could have a stroke, paralysis or speech and vision changes. If it is the kidneys, then you could have bloody urine and severe lower back pain. If it is the chest- the heart and the lungs, then you may feel breathless and have chest pain. If it is the abdomen, then you could have severe pain. Plus, your symptoms may be worse if you are dehydrated.
How To Diagnose And Treat Hypercoagulability?
Clotting disorders are normally diagnosed with detailed blood tests that look at clotting factors and various protein levels, along with a medical history and maybe a genetic assessment in rare cases. The blood tests can be basic or specific and check for various factors, along with antiphospholipid antibody testing. If you have DVT or related symptoms, then imaging may also be done.
As for medications and supplements to prevent blood thickening, anticoagulants are normally prescribed- like coumadin, heparin – which may be injected, or in the form of oral tablets – DOACs- direct oral anticoagulants. But all of these need regular monitoring to assess how you are responding to treatment. If it is too less or too much, then dosage will be adjusted as needed, by your doctor.
Best Lifestyle Changes To Reduce The Risk Of Hypercoagulability-
If there is a genetic component to your clotting disorder, then you don’t have much choice but to continue taking medications and adjust as necessary. But, making some lifestyle changes can make the whole transition much easier for you and your body. You should talk to a haematologist who will help monitor your condition and treatment. You should also be physically active everyday and eat well- so that your heart is not too strained. If you have other conditions like diabetes or hypertension, then you will need special care. If your symptoms are rather severe, then you may need more specialised therapy like hormone therapy or prolonged immobilisation.
Conclusion
Eating well, maintaining a constant weight and getting enough physical activity and sleep can greatly help improve your chances of dealing with clotting disorders. Clotting disorders are dangerous for pregnant women especially, as it can cause a miscarriage. If you have heart disease or have had traumatic injuries, then your chances of developing clotting disorders is much higher. Using compression stockings and not being sedentary can greatly help in general. Talk to your doctor for a better understanding of this condition and how your treatment can work for you.